It wasn’t that long ago that many, if not most people, expected to lose some or all of their teeth in their lifetime and reserve themselves to placing their teeth in a cup on the bedside table. When I started dental school almost 20 years ago, significant time was devoted in the curriculum to learning how to make partial and full dentures from senior faculty members who, pardon the pun, “cut their teeth” making false teeth for generations of patients. While many people are still suffering with partial or full edentulism (the condition of having missing teeth), the incidence is declining. In fact, between 1957-2012, there has been a 78% relative decline in edentulism in the United States [1]. This is likely due in no small part to the invention of modern titanium root-form dental implants in the early 1980’s [2].
With advancements in tooth replacement using dental implants, patients these days have more options than ever before to replace missing teeth and avoid wearing removable dentures. Historically in the 1980’s-2000’s, most dental implant surgery was performed “free hand” based only on conventional 2-dimensional x-rays. In other words, the surgeon could not actually visualize and evaluate a patient’s underlying bone to place an implant before actually doing the surgery! Sometimes if the site was not adequate, the surgeon and patient would discover (at the same time no less) an implant was either not possible or not possible without additional procedures. Other times, an implant would be placed, but in a poor position making attaching the actual prosthetic tooth difficult or impossible. Some clinicians may even still be practicing this way today.
A critical advancement in the field was the introduction of 3D cone-beam tomography that allows 3D visualization of the bony structures with less radiation than conventional medical CT scans [3]. We now have the ability to examine potential dental implant sites with high detail and accuracy. And before ever touching the patient, we can determine potential anatomical limitations as well as the ideal location for the dental implant. Most dental implant surgeons have been employing this technology since the 2010’s and it’s resulted in safer and more predictable tooth replacement than ever before.
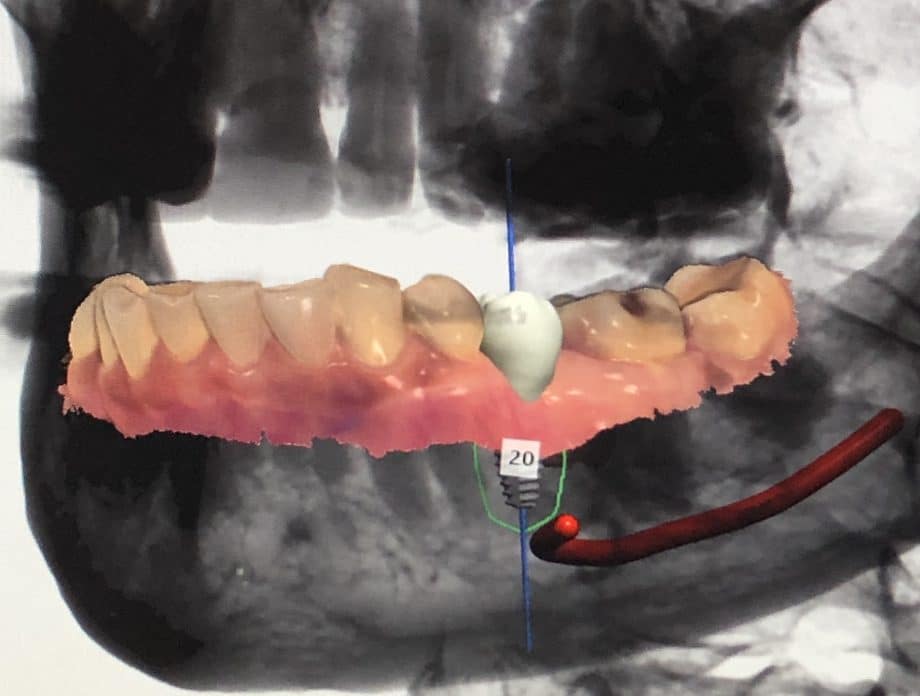
Today there is another equally critical advancement occurring. The introduction of optical intraoral scanning, dental CAD (computer assisted design) software and in office 3D printing is advancing this field even further. We now have the ability to fully digitize and virtualize a patient’s jaw structures including their tooth shapes, soft tissues and underlying bone structures. Data combined from the (radiation-free) optical intraoral scan and the 3D cone beam CT scan is used to precisely plan the ideal virtual position of a dental implant in software while avoiding vital structures like nerves and sinuses (figure 1). We then fabricate a custom 3D printed surgical guide stent for the implant surgeon right in the office that is used to accurately place the dental implant within 1mm of our virtual computer plan![4] This can be done for a single tooth or all of the teeth. The benefit of this exciting technology is we are treating patients quicker, safer, more predictably than ever. Many times, patients can even go home with temporary teeth on their implants the same day as surgery (figure 2). If only my denture professors could see what is possible today!
Figure 1
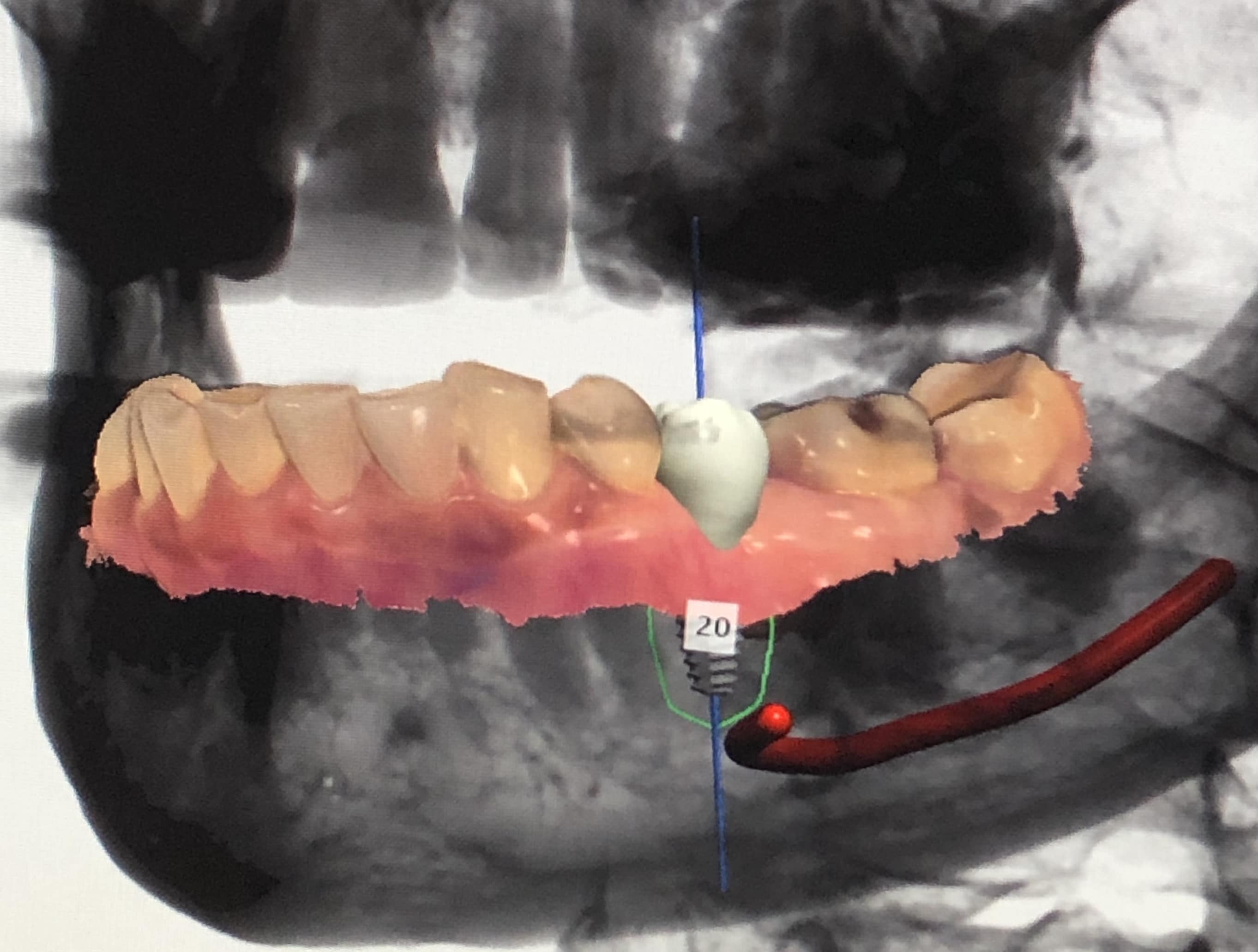
Figure 2

REFERENCES
- Projections of U.S. edentulism prevalence following 5 decades of decline.
Slade et al., J Dent Res. 2014 Oct; 93(10): 959-965. - A brief historical perspective on dental implants, their surface coatings and treatments. CM Abraham, Open Dent J. 2014; 8: 50-55.
- Patient radiation dose and protection from cone-beam computed tomography.
Gang Li, Imaging Sci Dent. 2013 June; 43(2): 63-69 - The accuracy of a 3D printing surgical guide determined by CBCT and model analysis. Ma et al, J Adv Prosthodont. 2018 Aug; 10(4): 279-285.